Neonatal cholestasis is defined as jaundice with high color urine staining diaper in an infant within first 3 months of life.
The common causes of neonatal cholestasis are –
- Extra hepatic – biliary atresia, choledocal cyst
- Intrahepatic – Idiopathic Neonatal Hepatitis (INH)
- Infectious – TORCH infection
- Metabolic – Galactosemia, Tyrosinemia, etc.
It should be kept in mind that Idiopathic Neonatal Hepatitis (INH) which is the most common cause of neonatal cholestasis is a diagnosis of exclusion. Its diagnosis can be confirmed only by excluding other causes of cholestasis and these children improve completely on follow up.
When to suspect Neonatal Cholestasis
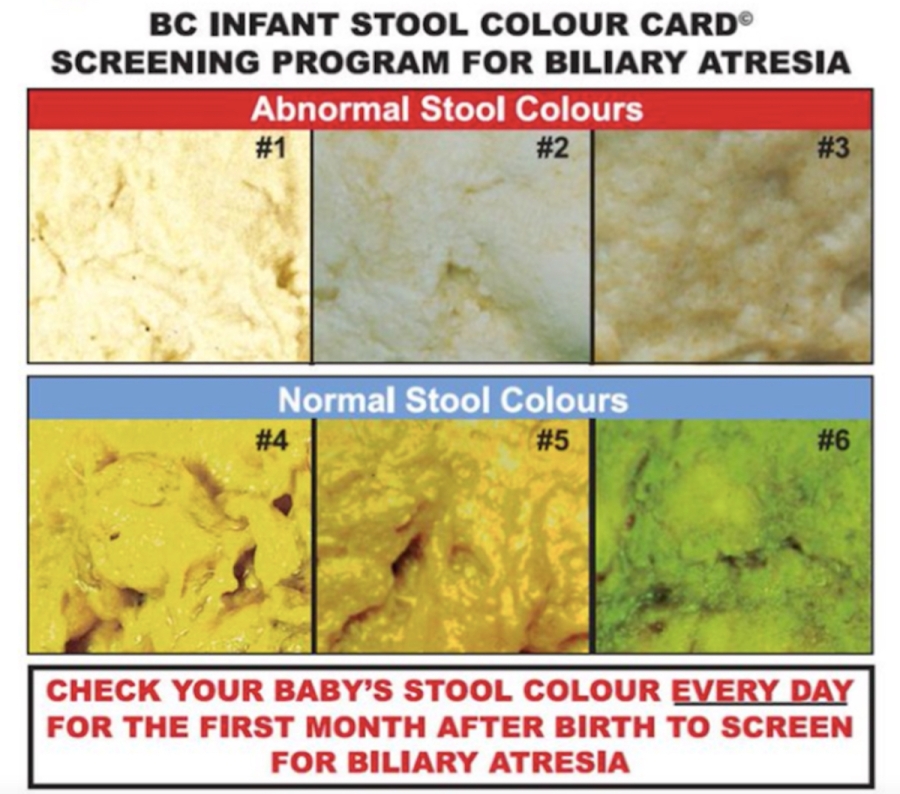
Any new born with jaundice and dark yellow urine staining the diaper with or without pale stools should be strongly suspected to have Neonatal Cholestasis.
Biliary Atresia usually presents with jaundice with diaper staining in an otherwise healthy well thriving baby.
Metabolic disorders commonly present with cholestasis with decompensation like bleeding, ascites and coagulopathy like galactosemia, tyrosinemia and neonatal hemochromatosis.
A detailed history and clinical examination helps to narrow down the differential diagnosis and focus investigation to confirm the diagnosis
While evaluating a child with neonatal cholestasis, the most important priority is to exclude biliary atresia and causes like galactosemia which needs early diagnosis and treatment.
Investigations in Neonatal Cholestasis
- Conjugated hyperbilirubinemia
- Serum direct /conjugated bilirubin concentration greater than 1.0 mg/dL if the total serum bilirubin (TSB) is <5.0 mg/dL or greater than 20 percent of TSB if the TSB is >5.0 mg/dL.
- Conjugated hyperbilirubinemia at any age in a newborn is pathological and requires evaluation.
- Serum transaminases(SGOT/AST & SGPT/ALT) are sensitive indicators of hepatocellular injury, but lack specificity and prognostic value.
- Gamma-glutamyl transpeptidase (GGTP) is a marker of biliary obstruction and is elevated in most cholestatic disorders
- Complete blood counts with PBF Cholestasis with hemolysis is seen in galactosemia, Coomb’s positive giant cell hepatitis etc.
- Ultrasound especially to rule out choledochal cyst.
- Urine non-glucose reducing substance (NGRS) can be used as a screening test in a suspected case of galactosemia – CLICK HERE TO READ POST ON GALACTOSEMIA
Role of HIDA scan in Neonatal Cholestasis
Routine use of HIDA scan should be discouraged in all cases of neonatal cholestasis. Infant with neonatal cholestasis with pale stool (abnormal stool) where possibility of biliary atresia is high, time should not be wasted for a HIDA scan.
In case of normally pigmented stool, there is no role of HIDA scan.
However, HIDA scan can be considered in the following situations in neonatal cholestasis-
- Infant with neonatal cholestasis with changing stool color (earlier pale stools and now pigmented stool)
- Neonatal cholestasis with ambiguous stool (stools which are not clearly pale or pigmented)
Excretory HIDA scan report rules out biliary atresia in these cases as it has very high negative predictive value (100%) for ruling out biliary atresia.
However, a non-excretory HIDA scan can be found in both biliary atresia and non-biliary atresia cases, as its positive predictive is only 56%.
Priming with phenobarbitone prior to HIDA is not recommended.
Priming with UDCA is preferable and is given for 3 to 5 days prior to HIDA scan is required.
Treatment of neonatal cholestasis depends on underlying etiology.
- Biliary atresia needs early Kasai porto-enterostomy, before the age of 3 months
- Galactosemia needs lactose free diet.
- Nutrition and supplementation of vitamins play an important role in neonatal cholestasis irrespective of the underlying cause. Supplementation of fat soluble vitamins (A, D, E, K) is important. Usually 1.5- 2 times of the Daily recommended doses are used for most of the Vitamins and minerals/nutrients.
DOSES OF VITAMINS AND MINERALS IN CHOLESTASIS
| Vit A | Oral | 5,000-25,000 IU/day |
| Vit D | Oral | 400- 1,200 IU/day |
| Vit E | Oral(Cap Evion 200/400IU) | 50-400 IU/day or 15-25 IU/kg/day |
| Vit K | Parenteral (im or iv) | 5mg monthly |
| Water soluble Vitamins | Oral | 1.5 -2 times RDA |
| Calcium | Oral | 20-100 mg/kg/day |
| Phosphorus | Oral | 25-50 mg/kg/day |
| Zinc | Oral | 1 mg/kg/day |
| Magnesium | Oral | 1 meq/kg/day |
| Elemental Iron | Oral | 5-6 mg/kg/day |
Every infant with cholestasis needs early referral to Pediatric Gastroenterologist for evaluation of under laying cause without delay.
Post Credits: Matter Drafted by Dr Mridul Chandra Das, Former Pediatric Gastroenterologist at BLK Centre for Child Health.

